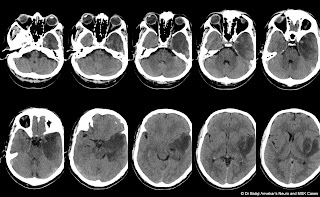
Clinical Details: middle-aged female, altered sensorium after convulsions.
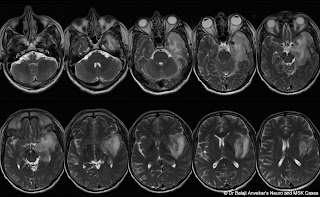
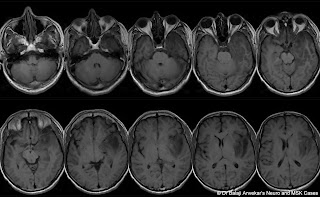
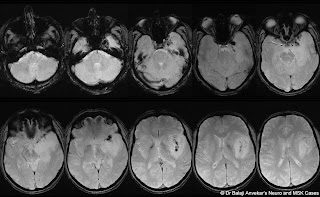
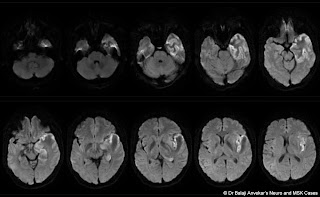
MRI study of brain shows:
Abnormal T2 hyperintensity with marked focal parenchymal swelling due to vasogenic oedema involving left temporal, insular cortex and adjacent opercular parietal white matter. An abnormal leptomeningeal enhancement depicted on post contrast MRI along left sylvian fissure and in left medial temporal region near cavernous sinus. Multifocal low signal intensity clustered nodularity in left sylvian fissure extending towards cavernous sinus on GRE which is hyper dense on CT. No abnormal calcification on CT. Normal MR angiography of brain. No obvious aneurysm or vascular malformation on MR angio.
Left side Decompressive hemicraniectomy done.
Intraoperative findings revealed thrombosed superficial cortical veins in left sylvian fissure region and at the floor of left middle cranial fossa.
Final diagnosis: Isolated superficial middle cerebral or Sylvian vein thrombosis.
Superficial middle cerebral vein also known as the Sylvian vein, is one of the superficial cerebral veins. It usually courses along the Sylvian fissure posteroanteriorly and drains numerous small tributaries from the opercular areas around the lateral sulcus. It curves anteriorly around the tip of the temporal lobe and drains into the sphenoparietal sinus or directly into the cavernous sinus.
Suzuki classification of the superficial Sylvian venous drainage pathways:1. sphenoparietal type: (54%) drains into the sphenoparietal sinus.
2. emissary type: (12%) courses along the lesser wing of sphenoid, turns inferiorly to reach the floor of the middle cranial fossa, joins the sphenoidal emissary veins, and passes through the floor to reach the pterygoid plexus.
3. cavernous type: (7%) directly drains into the anterior end of the cavernous sinus.
4. superior petrosal type: (2%) runs along the lesser wing and just before reaching the cavernous sinus, turns downward along the anterior inner wall of the middle cranial fossa, then runs along its floor medially to the foramen ovale to join the superior petrosal sinus.
5. basal type: (2%) runs along the lesser wing, turns downward along the anterior wall of the middle cranial fossa, then runs along its floor laterally to the foramen ovale over the petrous pyramid, presumably to join the transverse sinus through the lateral tentorial sinus or superior petrosal sinus.
6. squamosal type: (2%) turns directly backward along the inner aspect of the temporal squama and runs posteriorly to join the transverse sinus or lateral tentorial sinus.